the skin's microbiome: what it is and why it matters

the bottom line
As the body’s largest organ, the skin is colonized by diverse group of microorganisms, many of which are harmless or even beneficial. When this ecosystem of the skin is in balance, we have healthy, clear skin. But when the balance between host and colonizers is disrupted, the result can be acne, inflammation, or premature aging. Read on to learn more about the skin’s microbiome and how to keep it healthy.
first layer: what is the microbiome?
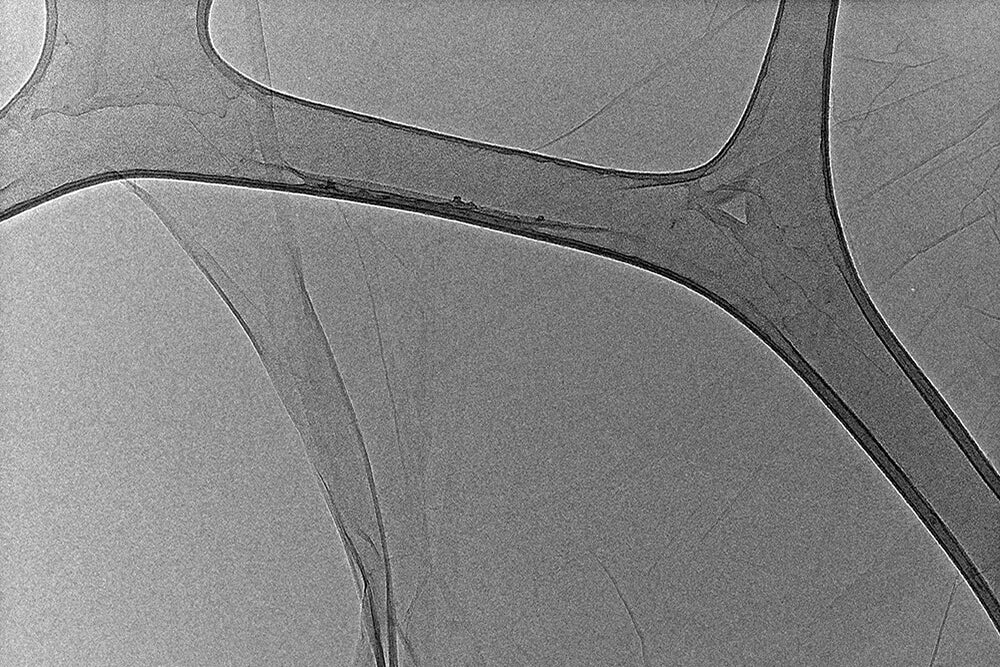
The skin’s primary role is to act as a physical barrier, protecting us from attack by foreign organisms and toxic substances. However, the skin can be considered to be its own ecosystem, with a number of living organisms that occupy their own diverse habitats. The habitat of the skin consists of invaginations and appendages such as sweat glands, sebaceous glands, and hair follicles.
The microbiome is the collection of microbes (bacteria, fungi, viruses, and their genes) that naturally occupy the ecosystem of the skin as well as the gut. Not only do they protect us against pathogens, but they also assist with development of the immune system and digestion. The human microbiome is incredibly diverse, with each body site possessing a different community of microbes. The microbiome of each of us is formed during the first few years of life, but can change in response to diet, medications, and environmental factors.
Because the microbiome sits between the body and the environment, it affects how we respond to specific environmental insults. Some microbes will make exposure to the environment more toxic, while others will protect the body. It’s currently believed that differences in the microbiome can lead to these varying responses as well as individual predispositions to illness. Environmental exposures can disrupt the microbiome and increase the risk of developing conditions including diabetes, obesity, allergies, and inflammatory bowel disease.
second layer: the science of the microbiome
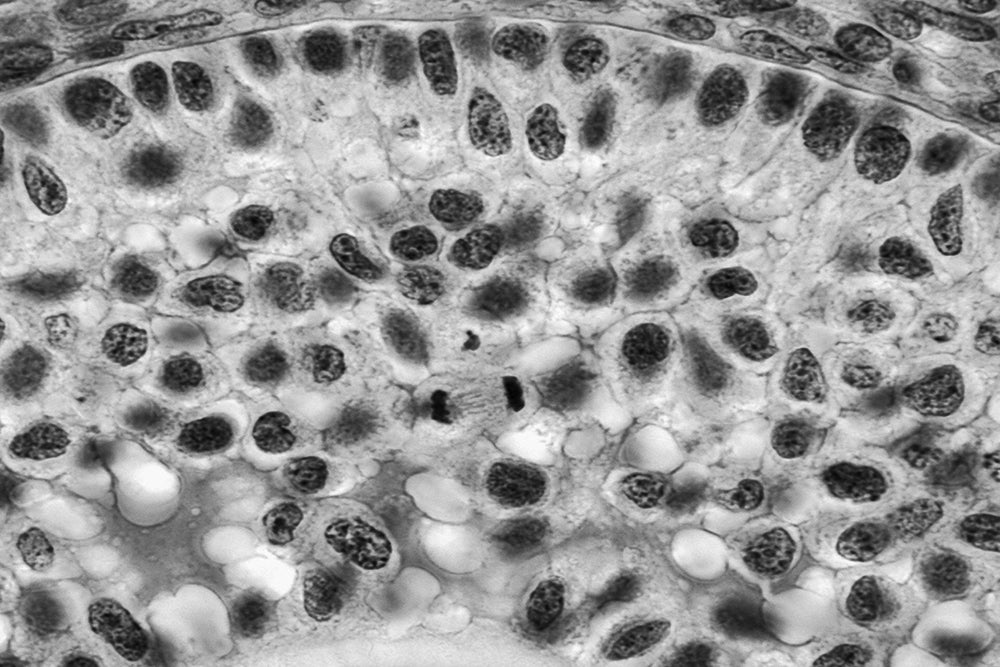
Most skin bacteria fall into one of four different groups: Actinobacter, Firmicutes, Bacteroidetes, and Proteobacteria. The proportions differ based on location, as Actinobacter are more common on the skin, while Firmicutes and Bacteroidetes are more frequently found in the gut. Propionibacterium species are predominant in sebaceous sites (such as the face and scalp), while Staphylococcus and Corynebacterium are more common in moist areas such as the umbilicus, armpits, and inner elbow. Temporal factors are also at play; when compared to the microbiome of the gut and the mouth, the microbiome of the skin has greater variability over time. Women have also been shown to harbor a greater diversity of bacteria on their hands as compared to men, although the reason for this is unknown.
In addition to presenting a physical barrier, the skin represents an immunological barrier. The immune response of the skin affects how we respond to wounds and infections. There are numerous microorganisms in the human microbiome which are related to pathogenic organisms or are themselves capable of becoming pathogenic. These include members of the genus Staphylococcus, Streptococcus, Enterococcus, Klebsiella, Enterobacter, and Neisseria. Staphylococcus epidermidis, a commensal* bacteria which lives on human skin, has been shown to modulate the host immune response by selectively inhibiting skin pathogens such as Staphylococcus aureus and Group A Streptococcus. When the skin’s immune response becomes deregulated, skin disorders such as psoriasis* and atopic dermatitis* can result. Seborrheic dermatitis*, a hyperproliferative skin disorder of the scalp associated with itching, has been associated with high levels of the fungus Malassezia. The preponderance of Propionibacterium acnes during puberty is associated with acne, while people afflicted with atopic dermatitis* are noted to be colonized with Staphylococcus aureus.
Chronic wounds are another example in which commensal bacteria become pathogenic upon breach of the skin barrier. While the bacteria do not cause the initial wound, they do contribute to the persistent inflammation and inability to heal which are characteristic of chronic wounds. Most wounds do not have a specific bacteria associated with them, but an exception is burn wounds, which are notably infected with Pseudomonas aeruginosa, Streptococcus pyogenes, or Enterococcus.
The microbiome and immune system of the skin communicate to help limit inflammation, with the immune system releasing various antimicrobial peptides when the balance of the ecosystem is lost. Similarly, the “good” bacteria on our skin can inhibit the release of inflammatory mediators from our immune system.
third layer: supporting the microbiome
Even in the presence of an excellent skin care routine, our skin may still be prone to inflammation and skin disorders because factors including environmental damage, skin pH, levels of oil production, and hydration status can all affect the individual microbiome. In general, it helps to create a diverse ecosystem in which there is a good balance of the various microbes.
Understanding that what we put into our bodies affects what we see on the skin, it’s critical to maintain a healthy diet and stay well-hydrated. Limit processed foods and extra sugar. Identify trigger foods and either decrease their quantities or eliminate them altogether. Dairy and gluten have both been associated with exacerbating skin conditions such as eczema and acne. There is current research which suggests that oral probiotics help to support a healthy gut and skin microbiome. Probiotics contain strains of live bacteria normally found on the skin, such as Lactobacillus and Bifidobacterium, and can help to reduce inflammation. Prebiotics are nutrients that help to feed beneficial bacteria, while postbiotics are the natural byproducts of bacteria living on our skin. Of course, regular exercise and controlling stress levels are also essential to maintaining a healthy gut and skin.
There are a few basic ways to protect and nourish the skin’s microbiome:
- gentle cleansing: avoid over-cleansing with harsh surfactants and sulfates which can strip the skin of essential oils and beneficial bacteria, exposing you to irritants and pathogens. consider using a cleansing oil to nourish and hydrate the skin prior to a creamy cleanser.
- balance the skin’s pH: keep in mind that our skin likes an acidic pH around 5.0. Cleansers tend to be alkaline and can disrupt the skin’s pH balance. Bring the skin back into balance with a hydrating toner.
- exfoliate: dead skin cell build-up on the skin’s surface can challenge the microbiome. Exfoliating twice weekly will help to remove dead skin cells, increase the rate of cell turnover, and improve the absorption of your other skincare products.
- nourish the skin barrier: hyaluronic acid, essential fatty acids, and ceramides help to nourish the skin barrier. Look for moisturizers and facial oils that contain these critical ingredients.
- protect: don’t forget the sunscreen. A mineral-based SPF of at least 30 creates a physical barrier which shields the skin from UVA and UVB rays and can help to calm inflammation. Use it every day, rain or shine.
fourth layer: how we do it
Supporting the skin’s microbiome is one of the most important ways to care for and protect your skin. We have a few favorites that can help:
- rice bran & pomegranate facial cleansing oil: a replenishing cleansing oil with rice bran, pomegranate, and castor seed oil to remove makeup, sunscreen, sebum, and sweat. All that good stuff that loves to clog pores.
- lotus flower & rosewater toner: a balancing toner made with botanical extracts of rosewater, lotus flower, gotu kola, and burdock root to cleanse and tone your skin. Balanced skin, bottled.
- jasmine serum: a hydrating serum that layers jasmine, sweet almond oil, and hyaluronic acid for glowy, glossy, glassy skin; gorgeous.
- bakuchiol & pomegranate facial oil: a luxurious facial oil that winds back wrinkles, with natural retinol alternative bakuchiol. It’s skin’s very own time machine. Fluorescent spandex not included.
- coming soon, our rosehip replenishing balm, with rosehip, sea buckthorn, mango butter, gota kola, and arnica. It’s a beauty balm for targeted renewal.
All this and more at www.anokhaskincare.com .
Add a layer by joining our newsletter: https://bit.ly/anokha_layers
xx
anokha
references:
- https://www.niehs.nih.gov/health/topics/science/microbiome/index.cfm#:~:text=The%20microbiome%20is%20the%20collection,to%20human%20health%20and%20wellness
- https://www.mindbodygreen.com/0-23996/your-skin-microbiome-why-its-essential-for-a-healthy-glow.html
- Grice EA, Segre JA. The skin microbiome. Nat Rev Microbiol 2011; 9(4): 244-253.
*definitions:
commensal: a relationship in which one organism derives benefits from the other without hurting or helping it
atopic dermatitis: a type of eczema remarkable for red, flaky, itchy skin, typically affecting the inner elbows and behind the knees. it's often seen with allergic rhinitis, hay fever, and asthma.
psoriasis: psoriasis is a skin disease characterized by a rash with itchy and scaly patches, typically found on the knees, elbows, trunk, and scalp.
seborrheic dermatitis: also known as dandruff, seborrheic dermatitis is an inflammatory, hyperproliferative skin condition marked by red, flaky skin on the sebaceous areas of the face, scalp, and trunk.
for more beauty definitions, explore the glossary.
faq's:
what is the skin microbiome?
the microbiome is the collection of microbes (bacteria, fungi, viruses, and their genes) that naturally occupy the ecosystem of the skin as well as the gut.
how do I restore the microbiome?
to support the microbiome, use a gentle cleanser, balancing toner, exfoliate dead skin cells, nourish the skin barrier, and protect with a sunscreen.
what is a healthy skin microbiome?
healthy skin has a balance of microbes within the skin's ecosystem.


leave us a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.